Overcoming alcohol problems: The good news (and the bad)
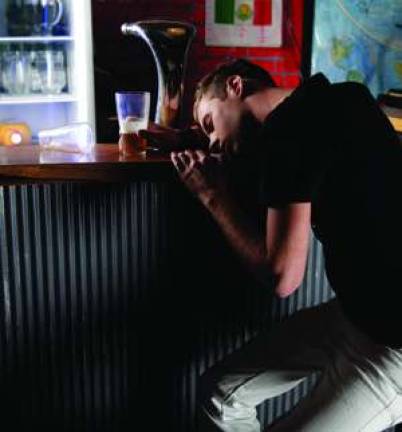
By David Gibbons The bad news is alcohol continues to be the most widely abused mood-altering, addictive drug in America, directly and indirectly responsible for billions of dollars in health care costs, crime and property damage-not to mention immeasurable lost productivity and personal devastation. Alcohol problems are widespread, and fewer addicts receive treatment in comparison to sufferers of other chronic conditions. A five-year study by Columbia University's National Center on Addiction and Substance Abuse (CASAColumbia), released this past June, found a huge treatment gap: As of 2010, there were 18.7 million Americans addicted to alcohol but only 1.7 million were treated. The study also revealed that of every government dollar spent on risky substance use and addiction, 96 cents paid for consequences and only 2 cents for prevention and treatment. Binge and heavy drinking are prevalent among alcohol users, especially the younger population (18 to 25), with figures of 50 percent and 25 percent, respectively, often cited. That's just some of the bad news; the statistics don't lie. But there is also plenty of good news. Organizations such as the National Institute on Alcohol Abuse and Alcoholism (NIAAA) and CASAColumbia are conducting much new research-covering both the effects of alcohol and the efficacy of treatments-and pushing for evidence-based reforms in health care and public policy. Counselors, therapists and clinicians continue to offer many options for heavy drinkers to curb their abuse and for alcoholics to achieve recovery. The research scientists are confirming much of what the psychologists have known all along: That along the spectrum of alcohol problems, there are multiple paths to recovery, and that a thorough individual evaluation, tallying genetic, psychological, environmental and other health factors and leading to a tailored treatment program, promises a more positive outcome. The medical profession has finally come to view addiction as a chronic ailment requiring long-term care and multiple treatment modes, including psychosocial and pharmaceutical. And it is establishing addiction medicine as a specialty-better late than never. The American Board of Addiction Medicine has accredited 10 residency programs, including one at The Addiction Institute of New York at St. Luke's-Roosevelt Hospital, and plans to double that number by early next year. More (qualified) good news: Based on its review of a 2001-2002 epidemiology study, the NIAAA concluded that most people who overuse alcohol do not become dependent. For those who do, it often starts in their early 20s and consists mostly of impaired control, as opposed to severe life-altering problems. After 20 years, three-quarters are in full recovery, i.e. they've either quit or cut down to low-risk levels; and fully 75 percent of these "recoverees" are able to do it on their own, without a formal support group or professional help. According to experts like Robert Huebner, Ph.D., deputy director of NIAAA in the Division of Treatment and Recovery Research, the "cure rate" for people with alcohol disorders is roughly the same as for other chronic diseases. One third achieve full remission, one third partial remission (significant improvement), and one third no improvement. For such a complex, stubborn affliction, apparently two out of three ain't bad. Nevertheless, the remaining third could no doubt benefit from more adequate treatment. On the spectrum of alcoholism, for those who "merely abuse" alcohol, moderation may be possible; for the addict, however, abstinence is the goal. In either case, relapses are common, and dealing with them is part of any good intervention or treatment program. The NIAAA publishes various pamphlets on the subject, including "Tips for Cutting Down on Drinking," which concludes with advice for alcoholics who want to quit altogether. Huebner and colleague David Goldman, M.D., chief of the NIAAA's Neurogenetics Lab, note scientists' increased understanding of individual and family predispositions toward alcoholism. For example, genetics can now identify people with a common variation that makes them susceptible to impulsivity and binge drinking-roughly 40 percent of us have it-so they can be forewarned before being exposed to cultural and environmental triggers. For individuals who become addicts, genetic profiling offers the promise of identifying which prescription medications will work for them. "If you're looking at alcohol alone, 50 to 75 percent of the risk that use becomes addiction is attributable to genetics," says Susan Foster, CASAColumbia VP and director of policy research and analysis. "But there are many other factors." She cites age of first use; co-occurring health conditions such as anxiety and depression; trauma; and multiple risk factors, for example, genetic predisposition combined with trauma. "Understanding these factors is very important in terms of helping people recognize what to look out for, the same as with other chronic conditions such as heart disease. It all gets back to asking, 'What's the nature of the problem and what's the best solution?'" At the Freedom Institute, a private outpatient facility in Midtown, addiction is treated as a family disease. "It affects everyone-not just the addict but all the family members who have been living with it and all the systems and patterns that have developed because of it," says Executive Director Donna Wick, a psychologist and expert on child development. "Recovery and relapse-prevention rates are substantially better when the whole family gets treatment. We've learned that the single best prevention for adolescent substance abuse is a close relationship with parents." Wick stresses that substance-use can alter young developing brains, before the age of about 25, so one of the main thrusts of their prevention efforts in schools is delaying first use. "If parents say, 'Well, we drank in high school,' I try to explain it this way: Our parents' generation didn't know smoking was dangerous. We know a lot more now than we did then." Anecdotal and scientific evidence as well as clinical experience consistently indicate what works best for addiction is a personalized, targeted, multi-pronged strategy that addresses all substances and behaviors. The debate whether addiction should be treated as a mental disorder or a physical disease has been rendered pretty much moot by the embrace of this integrated approach. Among its most articulate proponents is Arnold Washton, Ph.D., veteran addiction psychologist, author and founder of Recovery Options, a private practice with locations in Manhattan and Princeton, N.J. (Washton's website, www.recoveryoptions.us, is an excellent source of information and advice.) Washton and colleagues follow a personalized psychotherapeutic model, emphasizing patient motivation. "It would be hard to argue that individualized treatment wouldn't do better than a dogmatic, one-size-fits-all approach," he says, pointing to the NIAAA's Project MATCH, a two-part clinical study comparing different types of treatment. "They found whether you use cognitive behavioral therapy, motivational enhancement or 12-step facilitation, the results are about the same. But looking more closely at individual therapists, the study suggests the ones who were accepting, engaging and inspiring were more successful than those who would read their clients the riot act and bat them over the head with denial. So it turns out that the ideology or philosophy of the treatment is not so important as the spirit in which it's delivered. "My succinct advice for people looking for help would be to start slowly and easily," says Washton. "Find treatment that's tailored to your needs rather than a pre-formulated all-or-nothing program. Start by getting an assessment from a specialist, e.g. an addiction psychologist or psychiatrist, and move on from there." The bottom line is the therapist acts as the facilitator of recovery, but ultimately it's the patient who supplies the motivation and desire. For the addict, the full story goes like this: Using all of the tools now available, your doctor can help you get better, but you've got to want it and be prepared to follow what can be a long and at times rocky road to recovery.